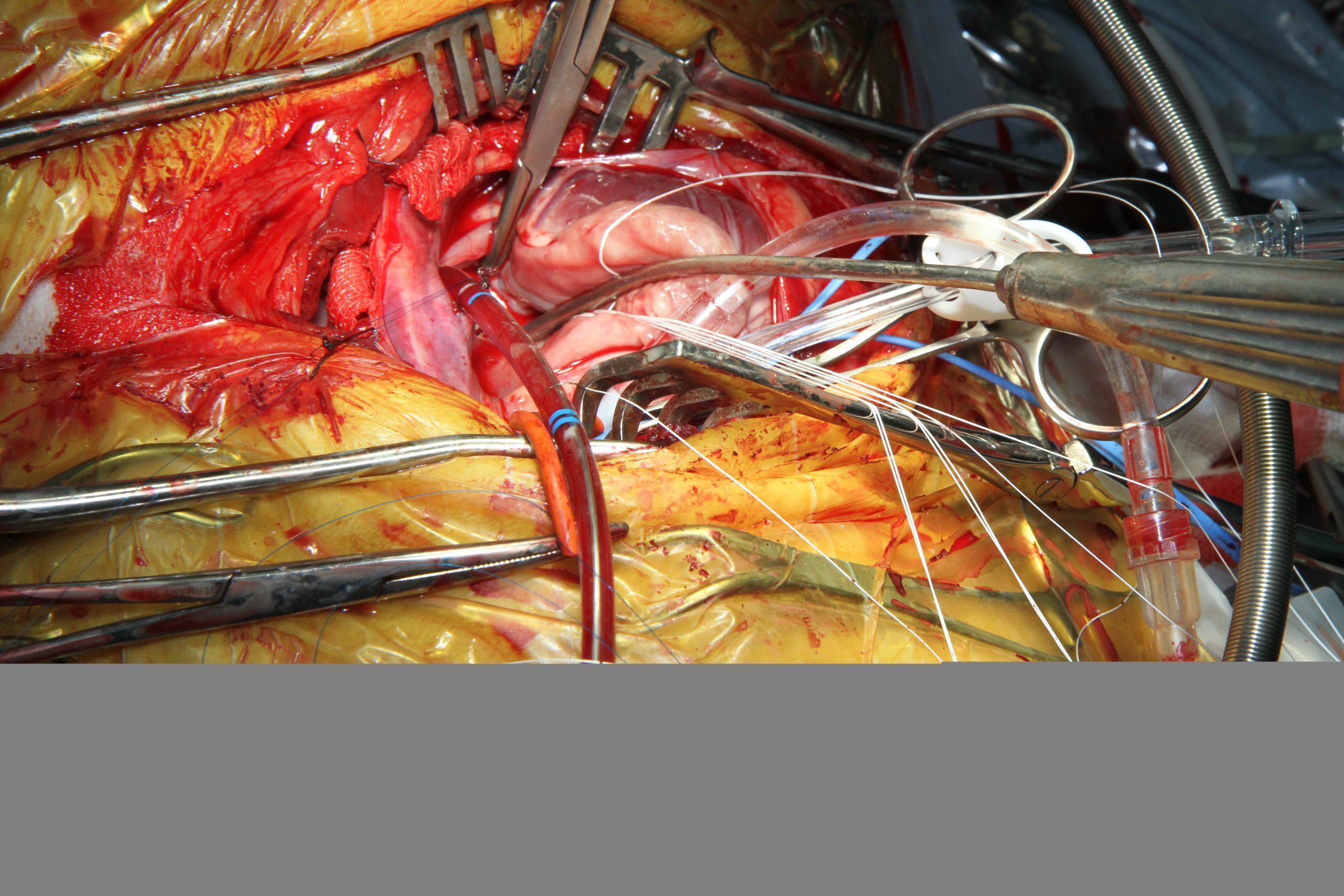
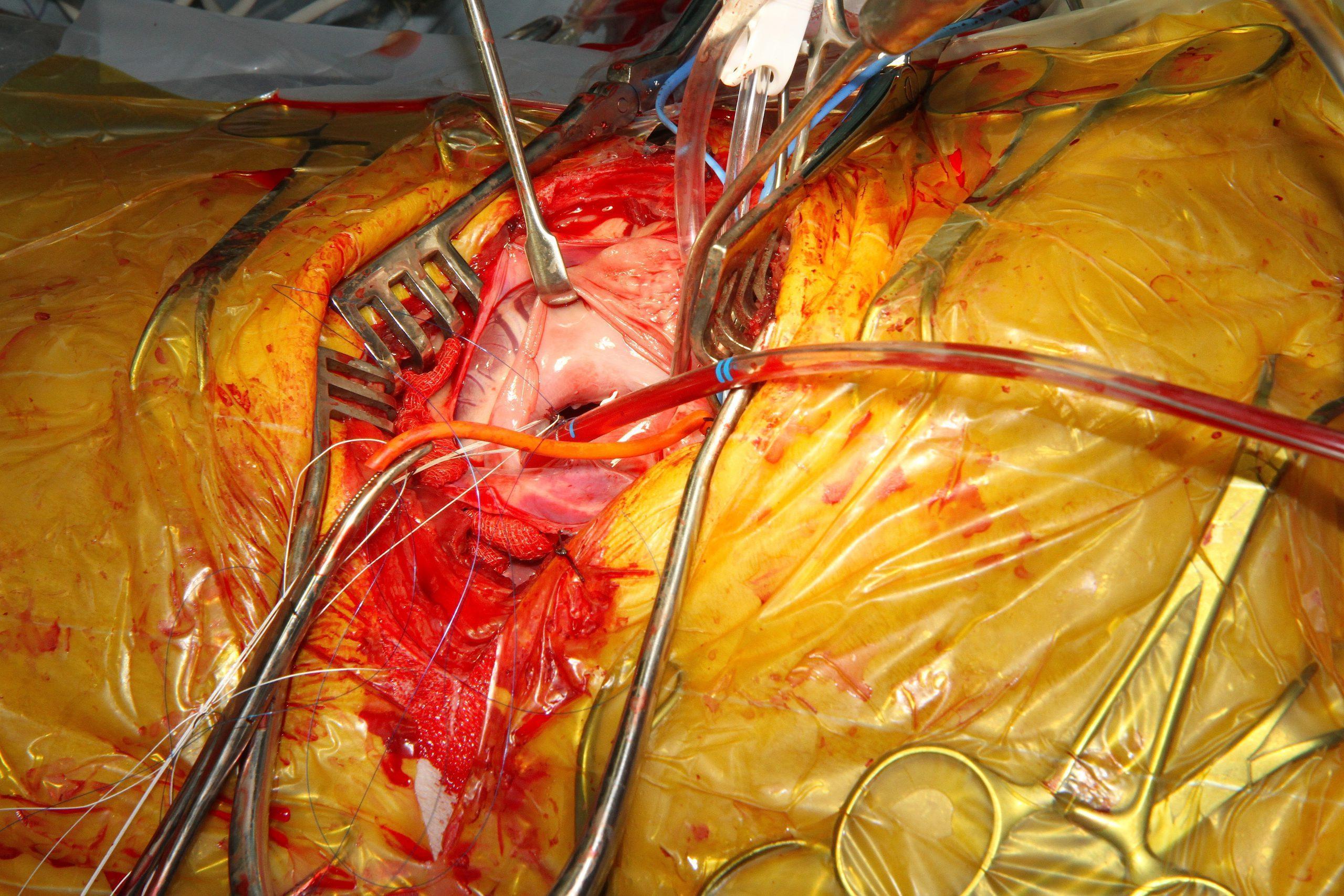
What better way to celebrate Valentine’s day than have your King Charles Spaniel’s Mitral Valve surgically repaired by our Austrian Cardio-surgeon “MacGyver” Dr. Peter Modler. Give the guy a few tubes, an ultrasound probe, a scalpel and a rock star surgical team & watch him do what was considered impossible only a short time ago; surgical repair the ubiquitously failing mitral apparatus from vegetative endocardiosis in a King Charles Spaniel. Dr. Modler, with the collaboration of rock star anesthesiologist Dr. Eva Eberspächer, DACVA, pulled a veterinary “MacGyver” move on this failing mitral valve with secondary left CHF and systolic dysfunction What better way to demonstrate the difference than with a cool series of echocardiograms on our February, 2015 SonoPath truly rock star case of the month. We are so very proud of you Peter! You and your collaborators are making history!
http://sonopath.com/about/specialists/peter-modler-dvm-dipl-tzt
*UPDATE: 3 weeks post surgery: What is the word for successful surgery and happy patient in Austria? Well there are 2 ways to say it…… “Super”… pronounced “Supaaahhhh” and “Wunderbar”! See why Peter is using these words 3 weeks after the surgical mitral valve repair on this stage C2 valve disease King Charles Spaniel. See the follow-up picture and video below.
**UPDATE: 2.5 years later Dr. Modler’s patient is alive and thriving. 🙂
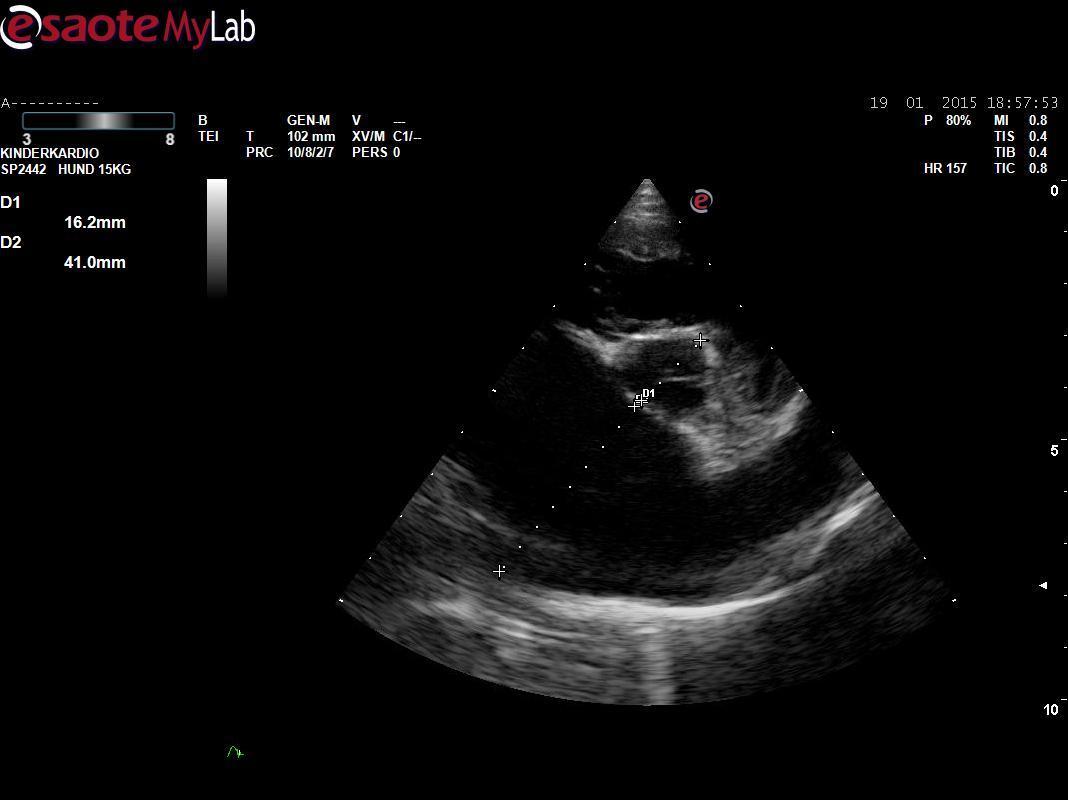
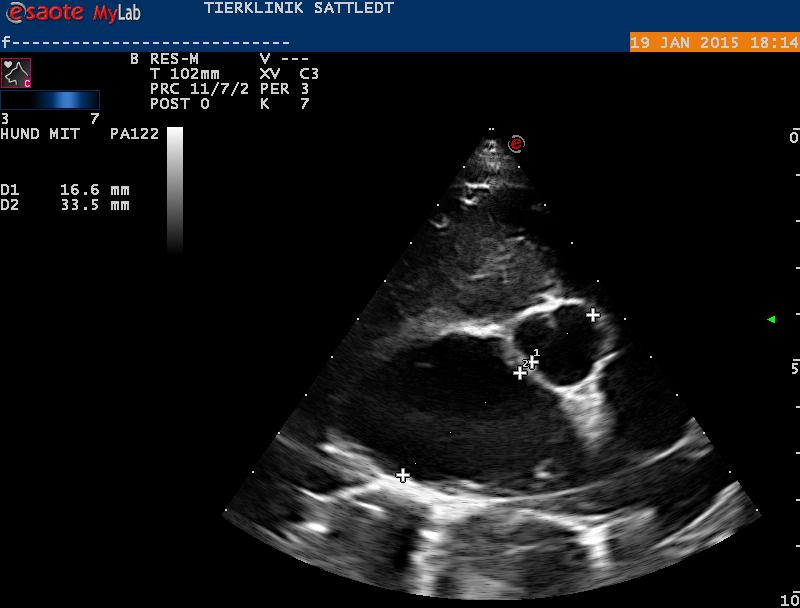
A 6-year-old MN Cavalier King Charles Spanial was referred for mitral valve repair because of severe DMVD. At that time he was already on Pimobendan, Furosemide (12 mg/kg/d) and ACEI. He presented with increased respiratory effort and mild pulmonary edema.
A 6-year-old MN Cavalier King Charles Spanial was referred for mitral valve repair because of severe DMVD. At that time he was already on Pimobendan, Furosemide (12 mg/kg/d) and ACEI. He presented with increased respiratory effort and mild pulmonary edema.
Because of his rapid deterioration and the poor prognosis with medical therapy alone, mitral valve repair under CPB was discussed with the owners. Even though the prognosis was guarded given the marked systolic dysfunction (large enddiastolic diameter in the face of severe volume overload, FS 38%, hyperkinesia of the septum, severe hypokinesia of the free wall) the owners decided for the surgery. The procedure was scheduled four weeks later. In the mean time Pimobendan was increased to tid, and Spironolactone was added. On the day of surgery, Henri still had some degree of pulmonary edema. Thus,Torasemide was given 6 hrs before surgery. Systolic dysfunction had increased and some ventricular runs were noted on the Sono-ECG. Open heart mitral valve repair was performed (mitral annuloplasty, chordal replacement with Gore-Tex) on cardiopulmonary bypass. Cross-Clamp time was 85 min. After clamp removal and electrical defibrillation the heart started spontaneously in a sinus rhythm and blood pressure was immediately restored. The patient woke up 5 hrs after surgery and was able to walk a short distance after 7 hrs.He is now doing quite well, starts eating and walks around in the yard. The mitral valve coadaption has increased with mild residual regurgitation. Systolic function is markedly impaired but is improving day to day.