Neoplasia, fungal disease, benefit of the doubt for the patient, and a well placed needle. Clinically, fungal disease looks and acts like neoplasia while sonographically fungal disease looks like neoplasia … and we typically see a heck of a lot more neoplasia here in the Northeast USA as opposed to fungal disease. Buuuuuuuuut… that’s why we have a needle and know how and where to place it. This case is a typical example of that concept. Don’t give a cancer diagnosis until you have a needle that says so…. I have run into this scenario hundreds of times in my career as surely you all have at one time or another if you have been around the veterinary block for a while. But there is nothing more exemplary of diagnostic efficiency and fairness to our patients than a needle in a lesion and a cytologist that’s prepared, pragmatic and ready to read it… of course unless you can get histopath but same difference. Take a look at this Intrapet Imaging case read by SonoPath and managed by Dr. Dan Zakai of Frederick Road Veterinary Hospital- that resided in a non fungal region but came up fungal in the dx when cancer was first on everyone’s differential list given the presentation. A 22 gauge needle and a couple of slides cost less than 10 cents while our choices cost a lifetime. Sonopath’s Educational Telemedicine (TM) layout provided as always in this July 2016 case of the month.
A 2-year-old FS Beagle mixed breed. Clinical findings: 2 chest nodules. Fever of unknown origin. Vomiting/diarrhea. Altered CBC/Chem/UA values: WBC 20,000. TP 8.3. BUN subnormal at 5. Globulins sl. Elevated. Coag-wnl. HWT-neg.
A 2-year-old FS Beagle mixed breed. Clinical findings: 2 chest nodules. Fever of unknown origin. Vomiting/diarrhea. Altered CBC/Chem/UA values: WBC 20,000. TP 8.3. BUN subnormal at 5. Globulins sl. Elevated. Coag-wnl. HWT-neg.
Cranial abdominal lymph node or pancreatic mass. Concurrent lung nodules. Suspect sarcoma or carcinoma.
Neoplasia, possibly pancreatic or round cell origin with pulmonary metastasis. Fungal disease, pancreatitis and pneumonitis.
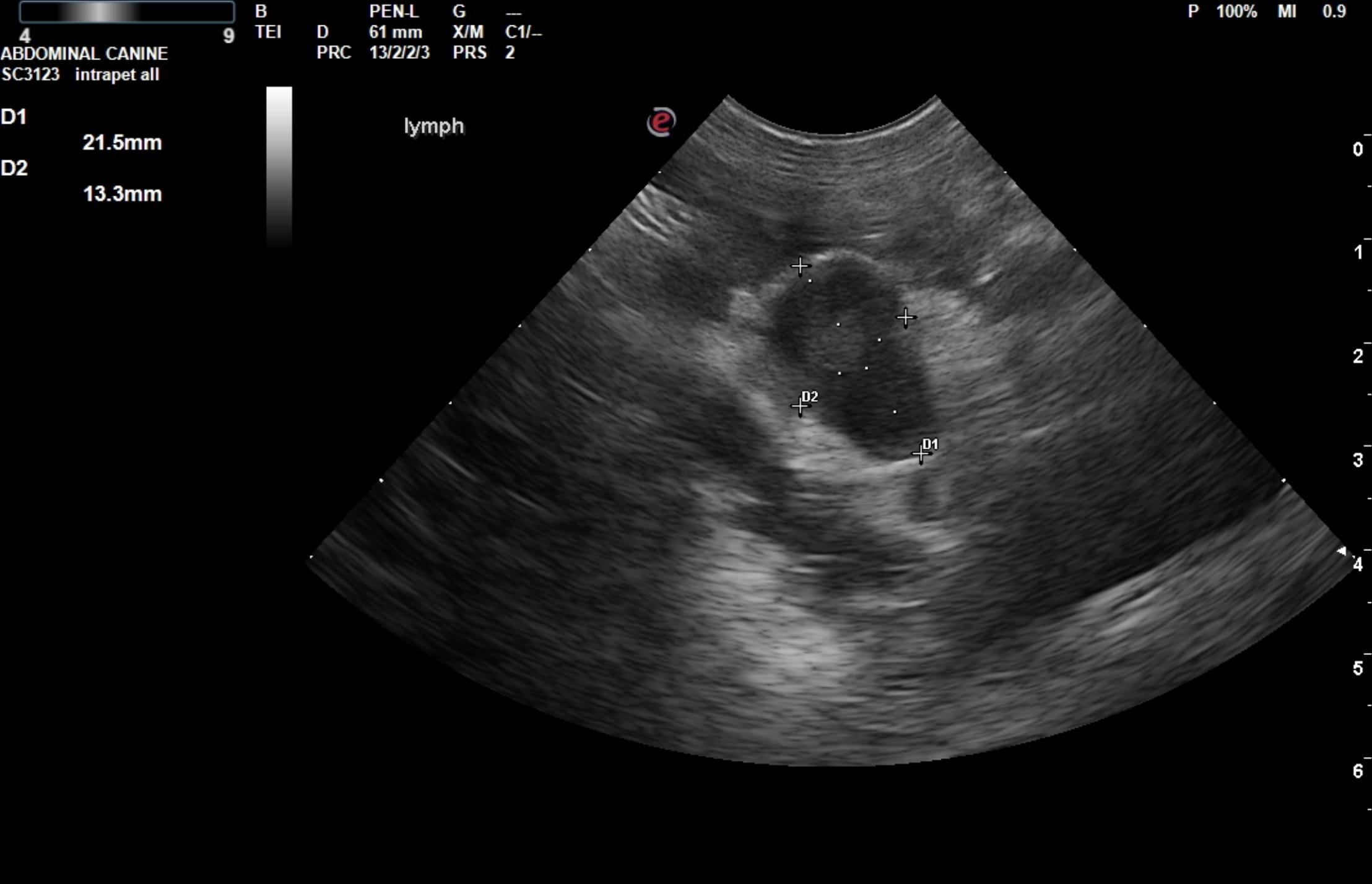
The gastric wall was slightly thickened in this patient. The remainder of the intestinal tract was unremarkable. The mesenteric lymph node was enlarged with distorted architecture and a pericapsular inflammatory pattern. The lymph node measured 2.15 x 1.3 cm with similar echogenicity to the lung nodules. A regional, mixed, hypoechoic area in the pancreas was also noted in this patient creating a 2.0 x 2.0 cm mass. This is likely of pancreatic origin or overlying distorted lymph node.
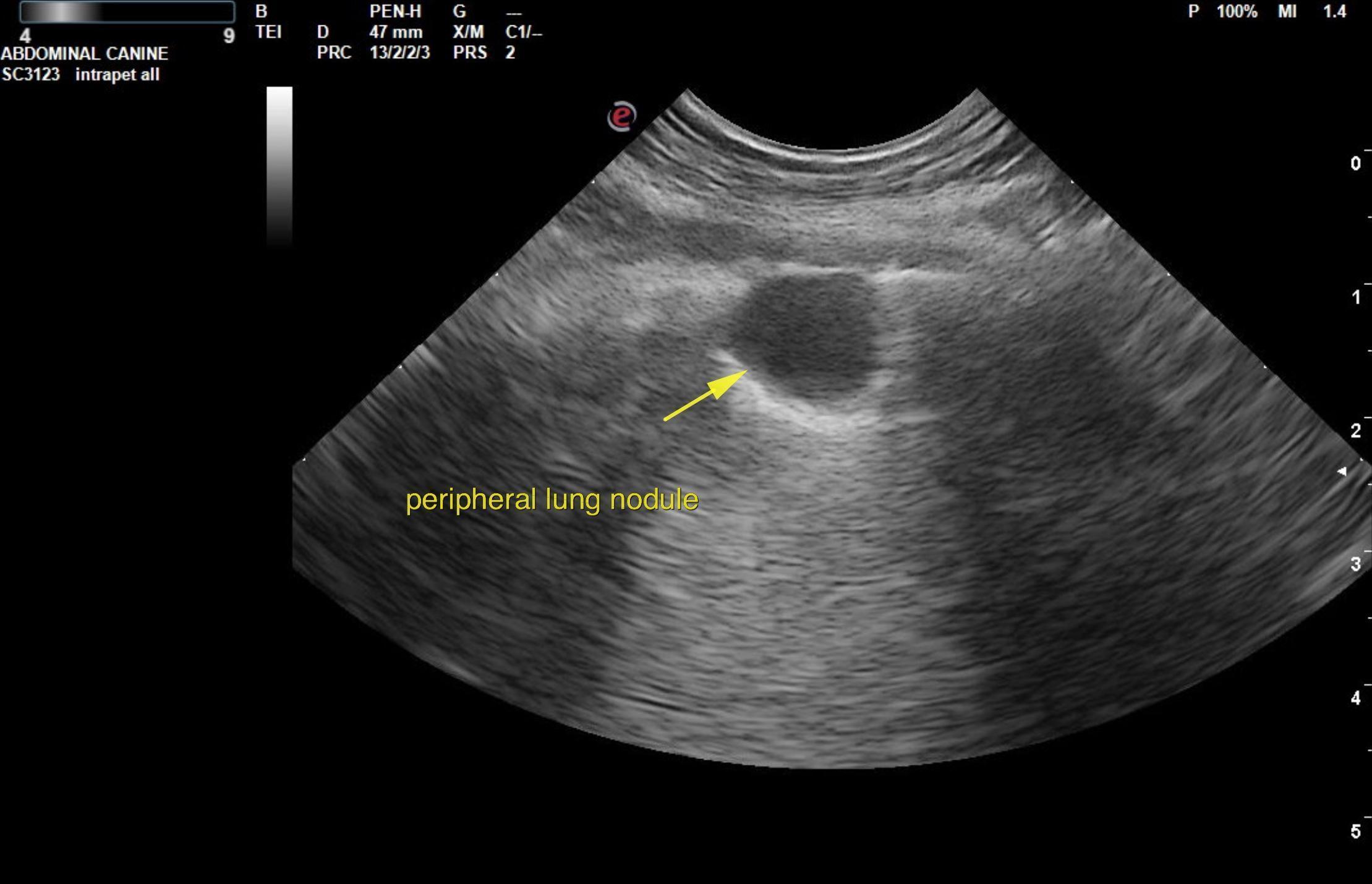
Thorax: The left thorax in this patient revealed a hypoechoic lung nodule that measured 1.25 x 1.09 cm. lung origin is confirmed by the peripheral air interface in the lesion.
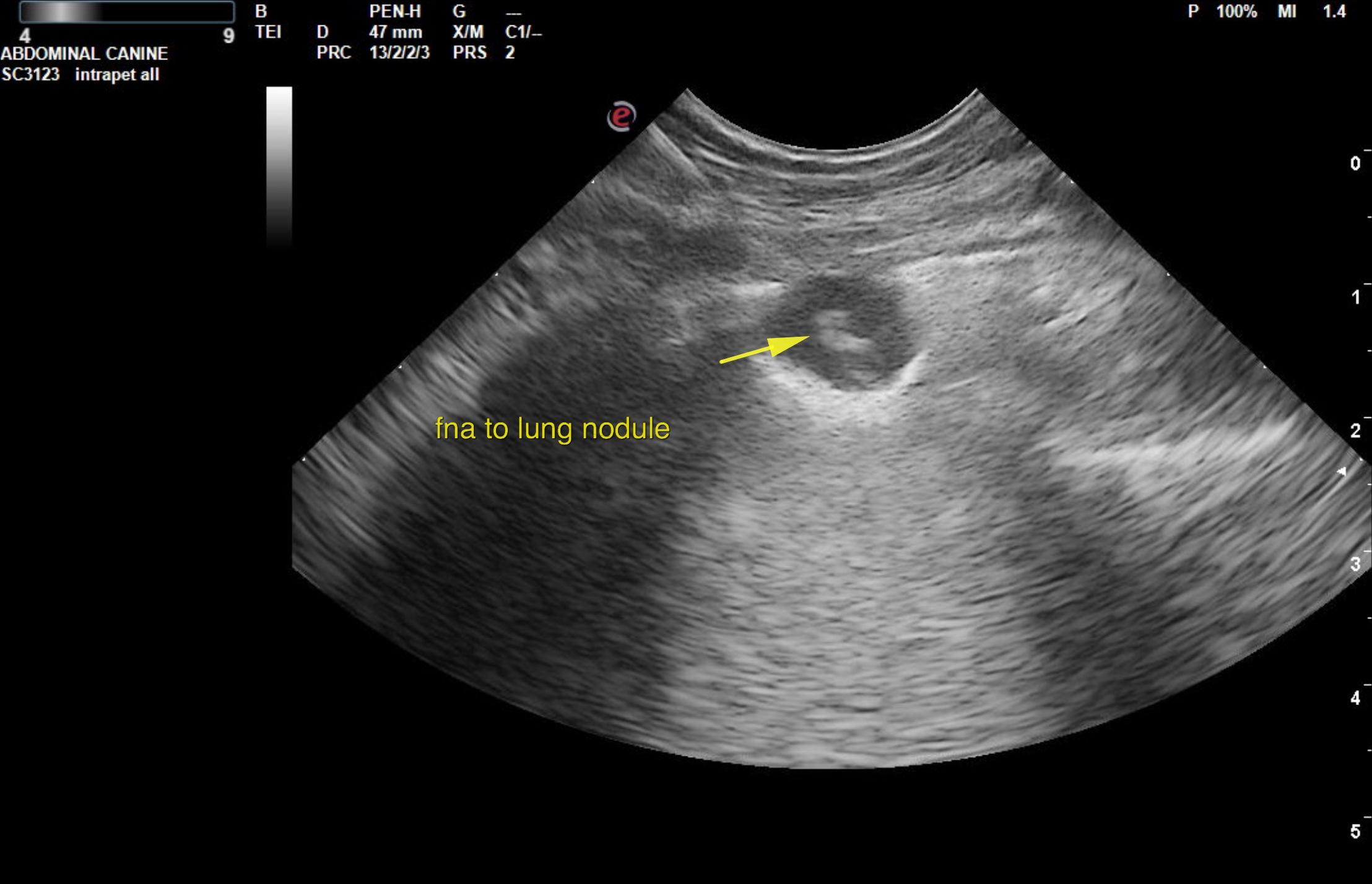
Ultrasound-guided FNA of the lung nodules were performed without complication. FNA of the mass in the region pancreas would have been ideal in this patient. U/S-guided FNA of the lung nodule revealed blastomycosis. The patient lived in a blast-free region for > 1 year but had been adopted before that so the origin of infection was likely from prior residence in a blasto endemic region.