The patient was presented for a pre-surgical cardiac evaluation. The patient was suffering from a rapidly progressing degenerative mitral valve. At the time of presentation the patient was on a regimen of Furosemide (8mg/kg/SID), Pimobendan (0.25 mg/kg/BID), Benazepril (0.25 mg/kg/SID), and Spironolactone (2mg/kg/SID). Despite her treatments, she was still experiencing exercise intolerance, mildly increased resting respiratory rate, and was coughing.
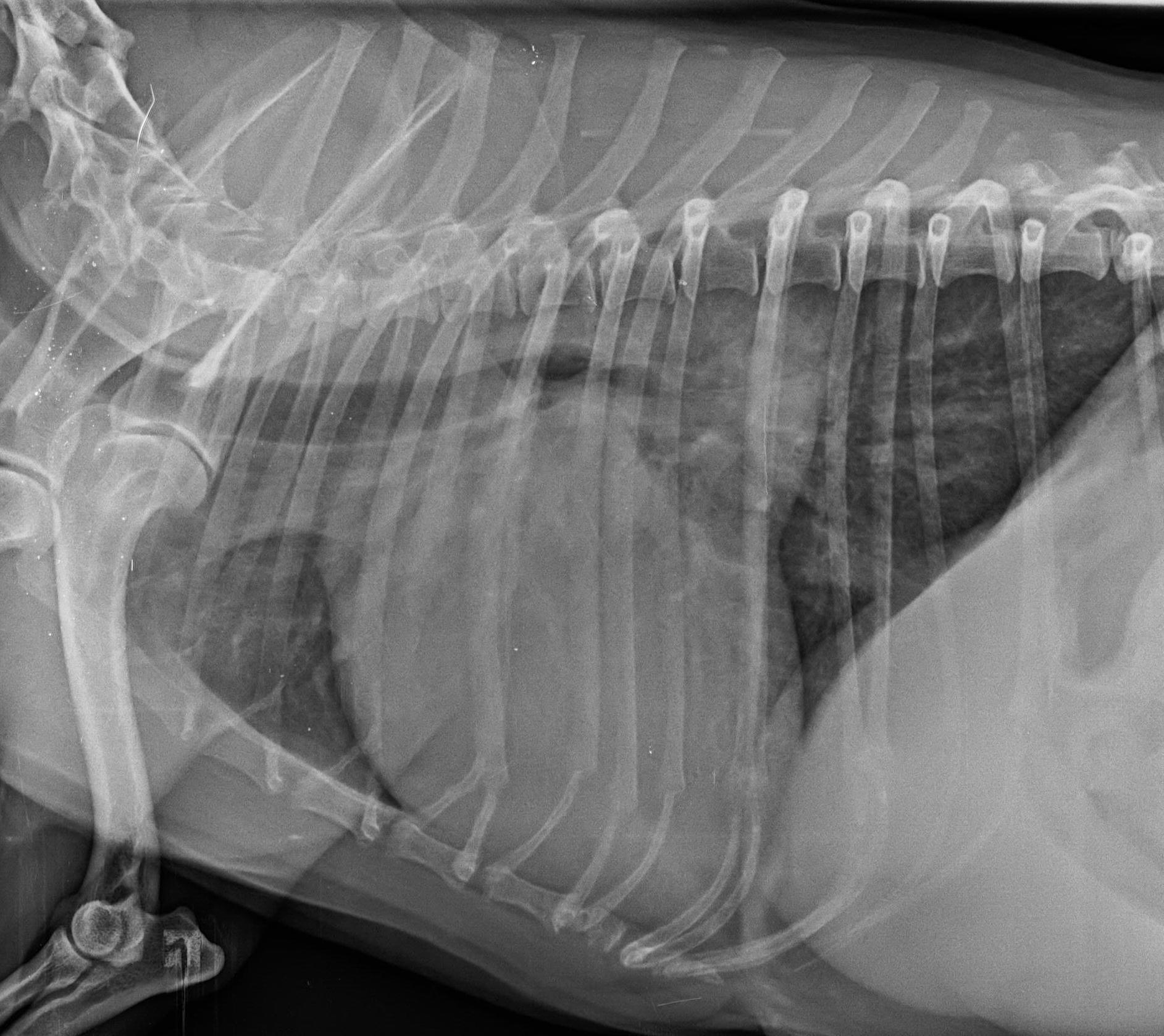
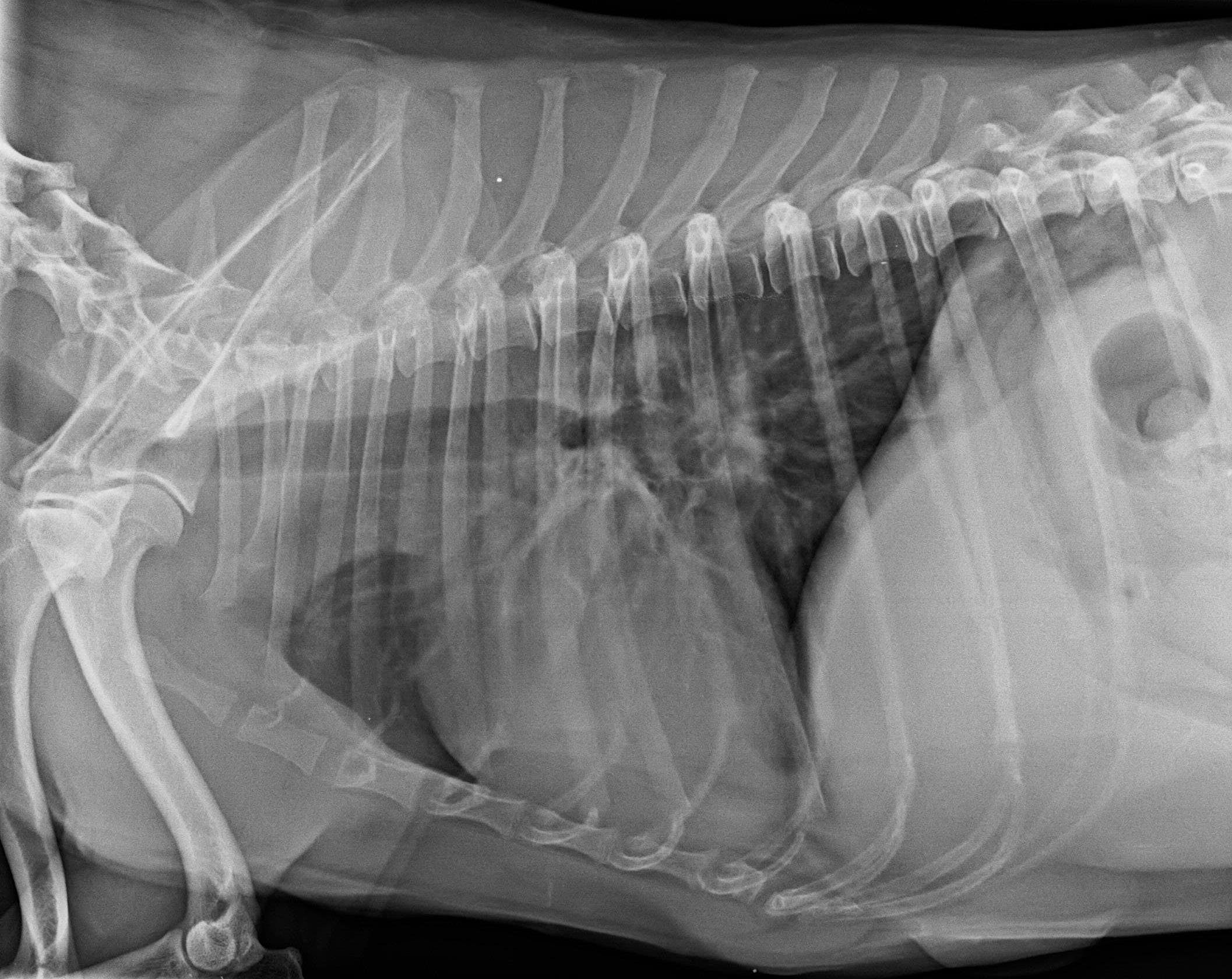
The patient was presented for a pre-surgical cardiac evaluation. The patient was suffering from a rapidly progressing degenerative mitral valve. At the time of presentation the patient was on a regimen of Furosemide (8mg/kg/SID), Pimobendan (0.25 mg/kg/BID), Benazepril (0.25 mg/kg/SID), and Spironolactone (2mg/kg/SID). Despite her treatments, she was still experiencing exercise intolerance, mildly increased resting respiratory rate, and was coughing. Thoracic radiographs showed severe cardiomegaly, an increased lung opacity due to a bronchio-interstitial pattern, elevation of the trachea with possible left mainstem compression (possible airway collapse) and mildly dilated pulmonary veins.
Rapidly progressing degenerative mitral valve.
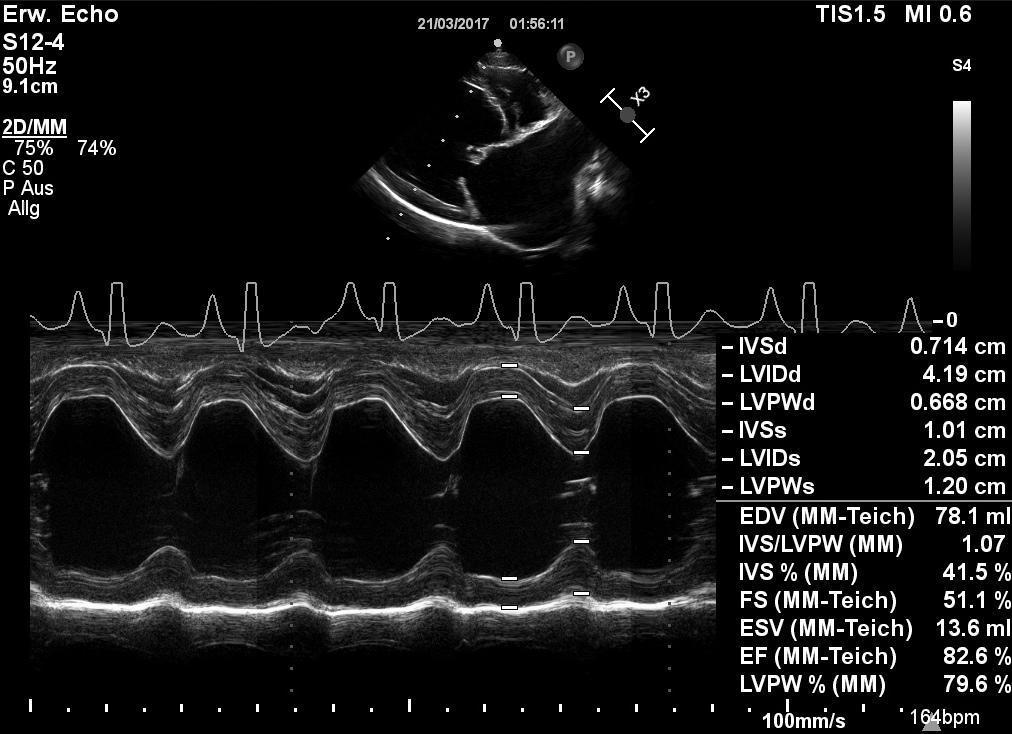
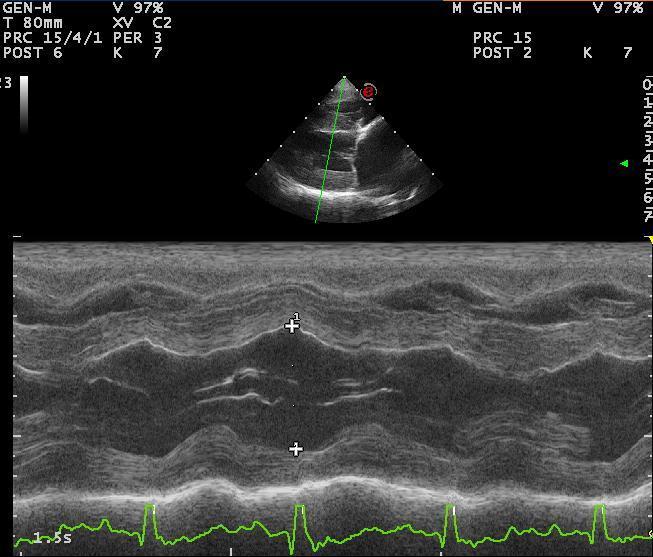
The left ventricle appeared severely dilated. However, systolic function seemed to be only mildly impaired. Both mitral valve leaflets showed a significant prolapse and thickening. Chordal rupture affecting the anterior leaflet was visible. The left atrium was severely enlarged. Mitral inflow profiles revealed significantly increased filling pressures and volume overload. Mild tricuspid regurgitation due to valvular degeneration was also visible. Systolic pressure gradients across the tricuspid valve indicated moderate pulmonary hypertension (50 mm Hg).
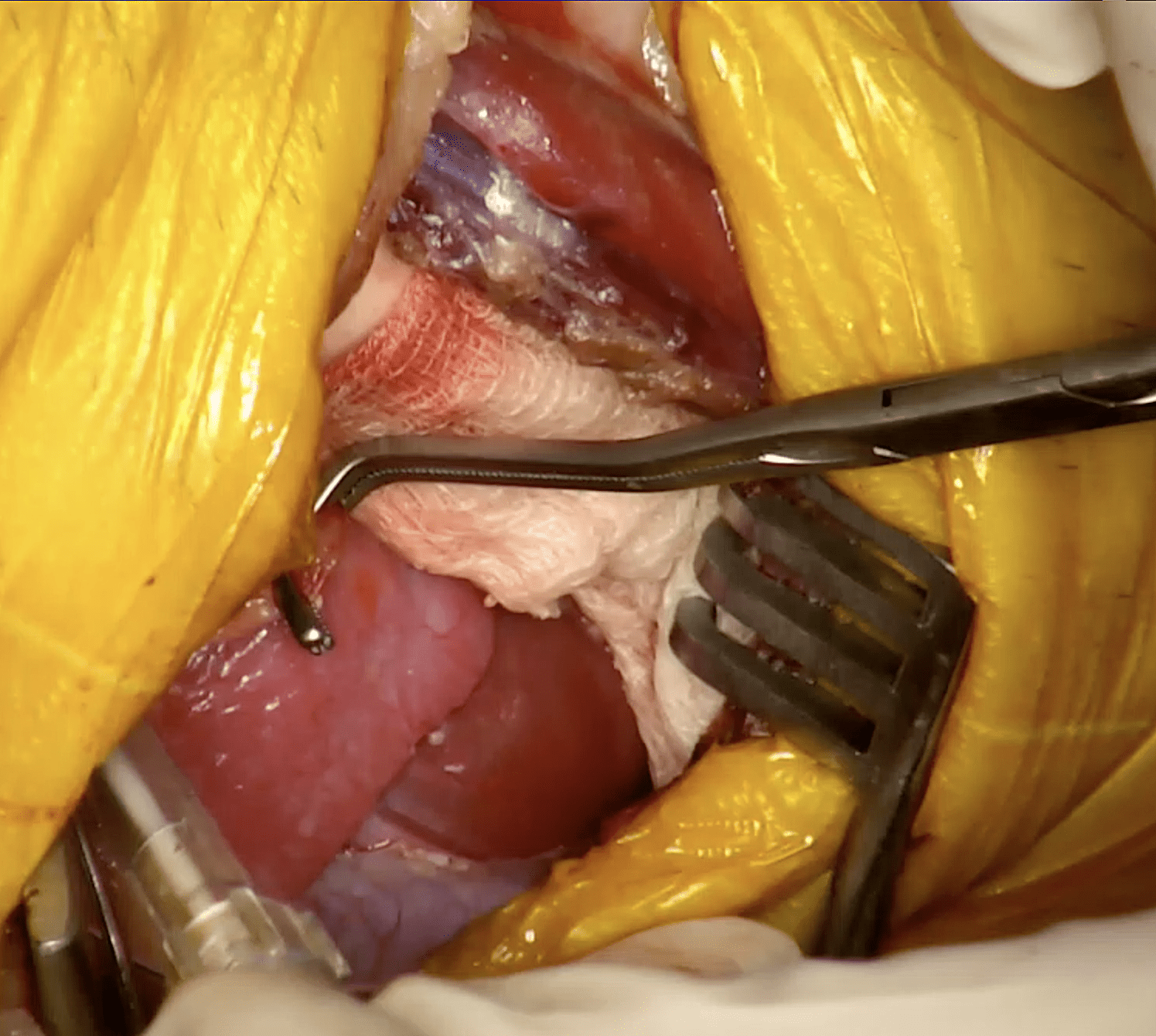
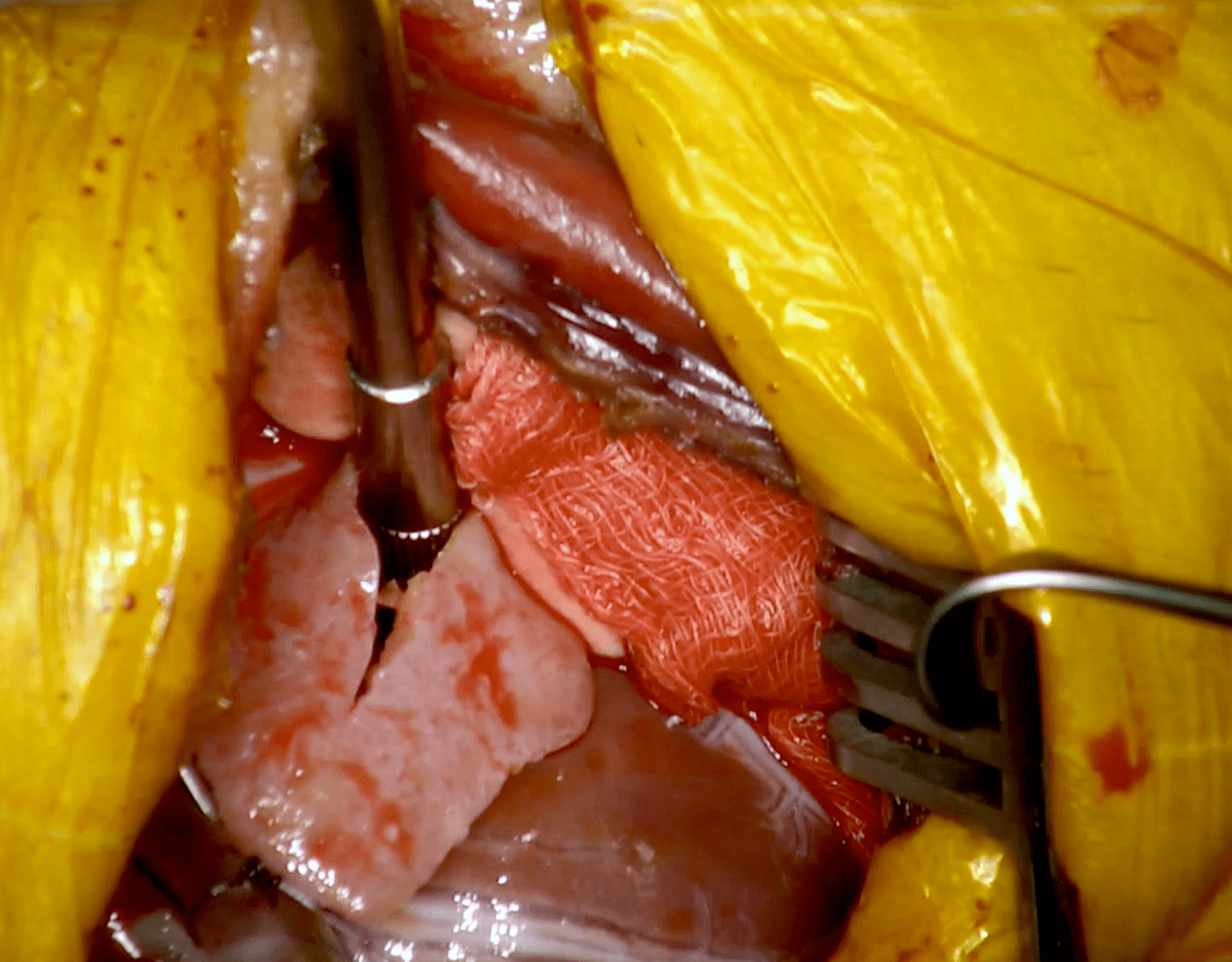
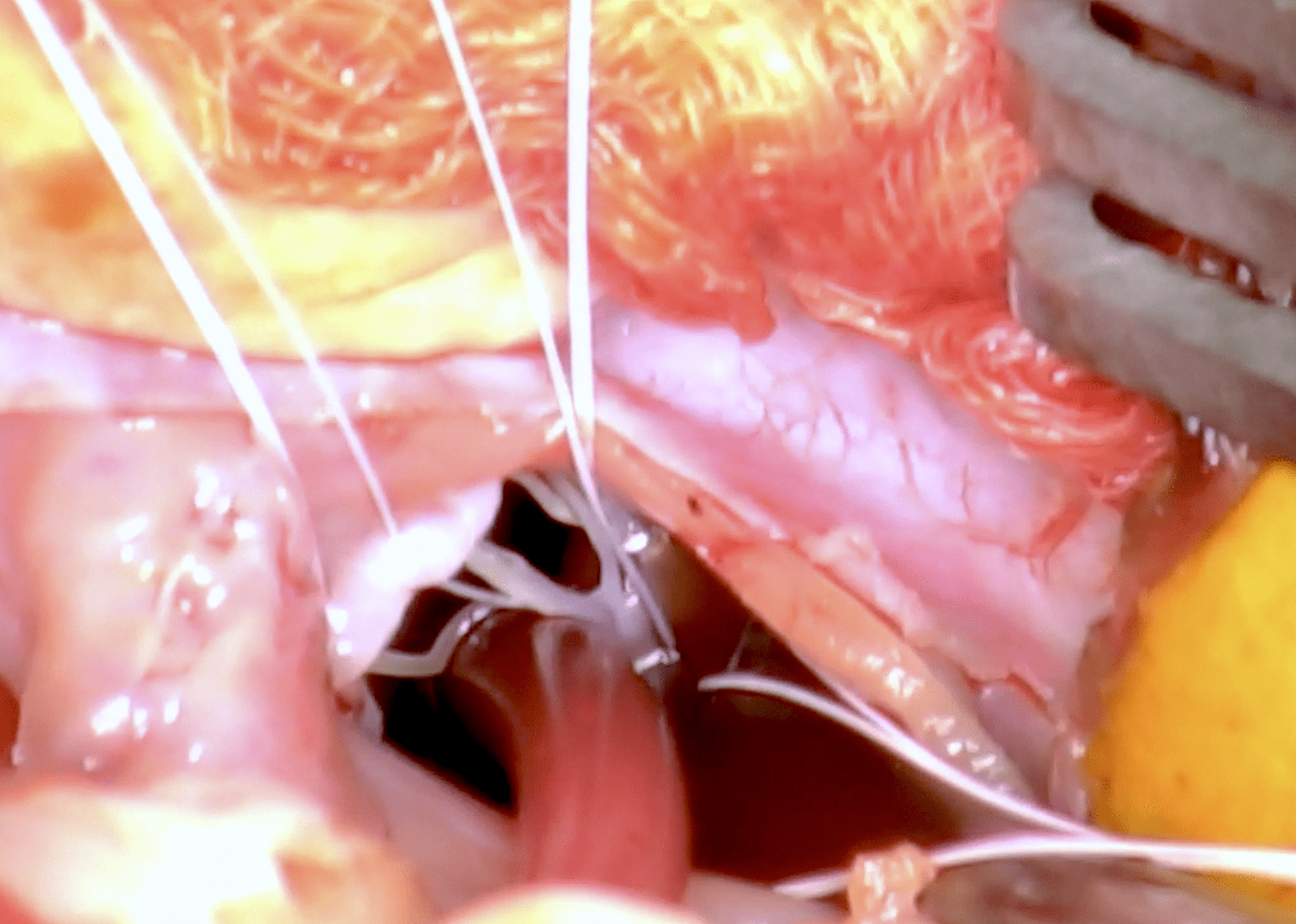
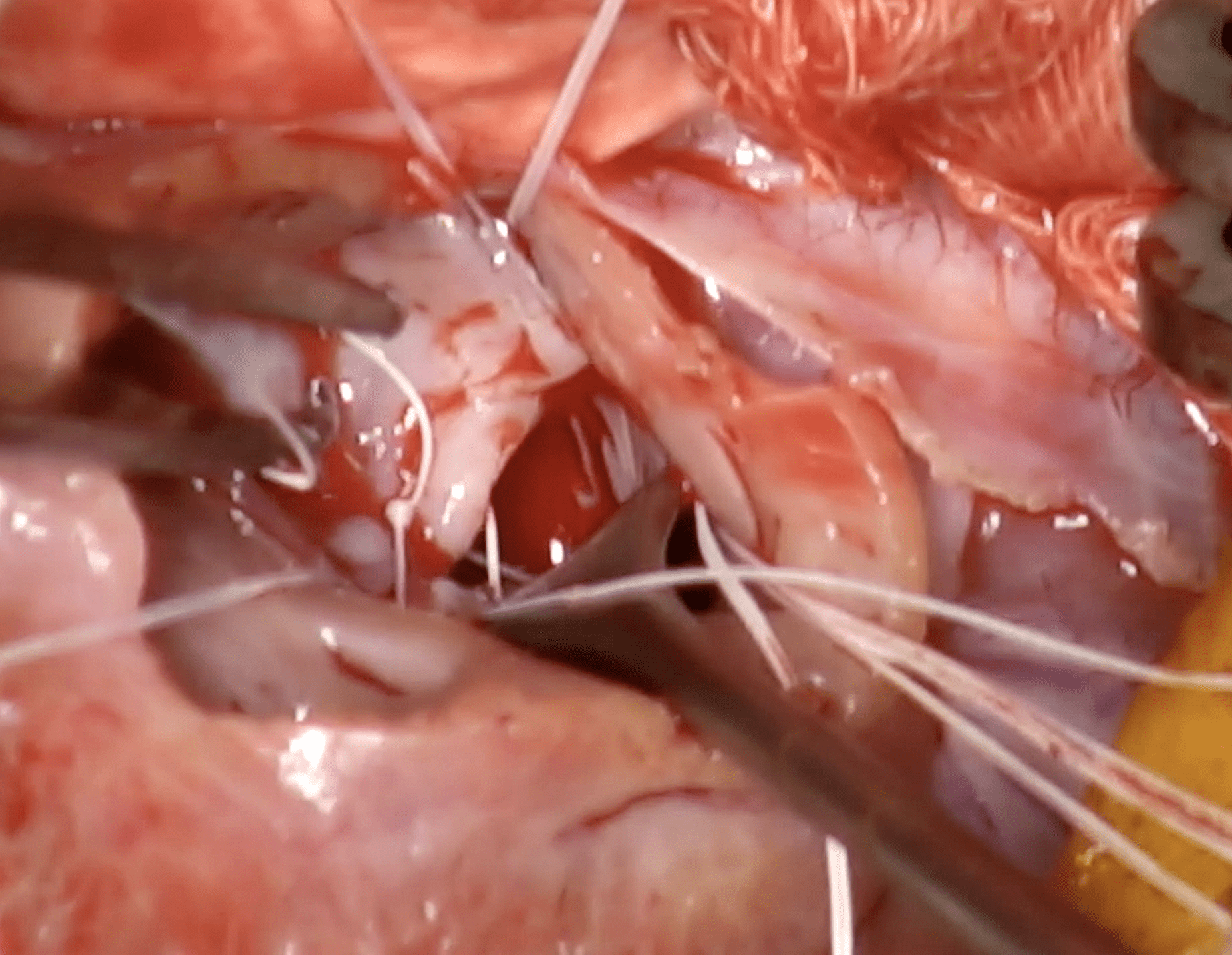
Open heart mitral repair was performed with the patient connected to an extracorporal circulation (heart lung machine). First, the cervical vessels (carotid artery and jugular vein) were prepared for cannulation. Next, a left 5-intercostal thoracotomy was performed and the pericardium was opened. The aortic root was freed from surrounding fat and prepared for insertion of the cardioplegia cannula. After administration of heparin, the cervical vessels were cannulated and connected to the extracorporal circuit (partial bypass). The cardioplegia cannula was inserted into the aortic root, followed by cross-clamping of the aorta and instillation of the cardioplegic solution (potassium solution for initiation of cardiac arrest and myocardial protection – full bypass). The left atrium was opened and suction tubes were inserted. After thorough inspection of the valve leaflets, artificial chordae were attached to the papillary muscles and then passed through the leaflet margins. A circumferential annuloplasty was performed in order to obtain an appropriate annular size. Therefore, pledgets were used to prevent the sutures from rupturing through the annular tissue. Afterwards, the chordae were adjusted to the appropriate length and tied. The left atrium was closed, vented, and the cross-clamp was removed. After a few seconds, the heart started with rhythmic contractions. The bypass was reduced and finally stopped, the cannulas were removed and hemostasis was re-established with protamine. Finally, the chest was closed over a chest drain which remained in place for the first 12 hours. The patient woke up uneventfully and was able to walk 5 hours after the end of surgery. Post-surgical echo showed good cardiac function and only mild mitral regurgitation. After more than 9 months post-op, the patient is still doing well.