Labored breathing is a common presenting complaint in small animals. Small breed dogs with a murmur pose a particular challenge, as these breeds are predisposed to both cardiac and respiratory pathology. Congestive heart failure is the most common reason for dyspnea, however pulmonary hypertension and concurrent respiratory disease must also be considered. Treatment for CHF can actually worsen clinical status in these cases, and differentiating the cause of dyspnea is crucial to selecting successful therapy. Pulmonary hypertension is a challenging diagnosis that is often overlooked or not apparent on thoracic radiographs, and echocardiography is the ideal tool to document this type of pathology.
We present a case of severe pulmonary hypertension in a Yorkshire Terrier that was initially treated for CHF.
Fabulous images provided by Andi Parkinson, BS, RDMS, owner of Intrapet Imaging and this case was expertly read out by SonoPath specialist Maggie Machen Lamy, DVM, DACVIM (Cardiology).
History: Presented to the ER for difficulty breathing. History of a collapsing trachea and chronic cough. Radiographs showed cardiomegaly with questionable pulmonary changes. Placed in oxygen and treated for CHF (lasix, pimobendan, hydrcodone) but did not do well.
History: Presented to the ER for difficulty breathing. History of a collapsing trachea and chronic cough. Radiographs showed cardiomegaly with questionable pulmonary changes. Placed in oxygen and treated for CHF (lasix, pimobendan, hydrcodone) but did not do well.
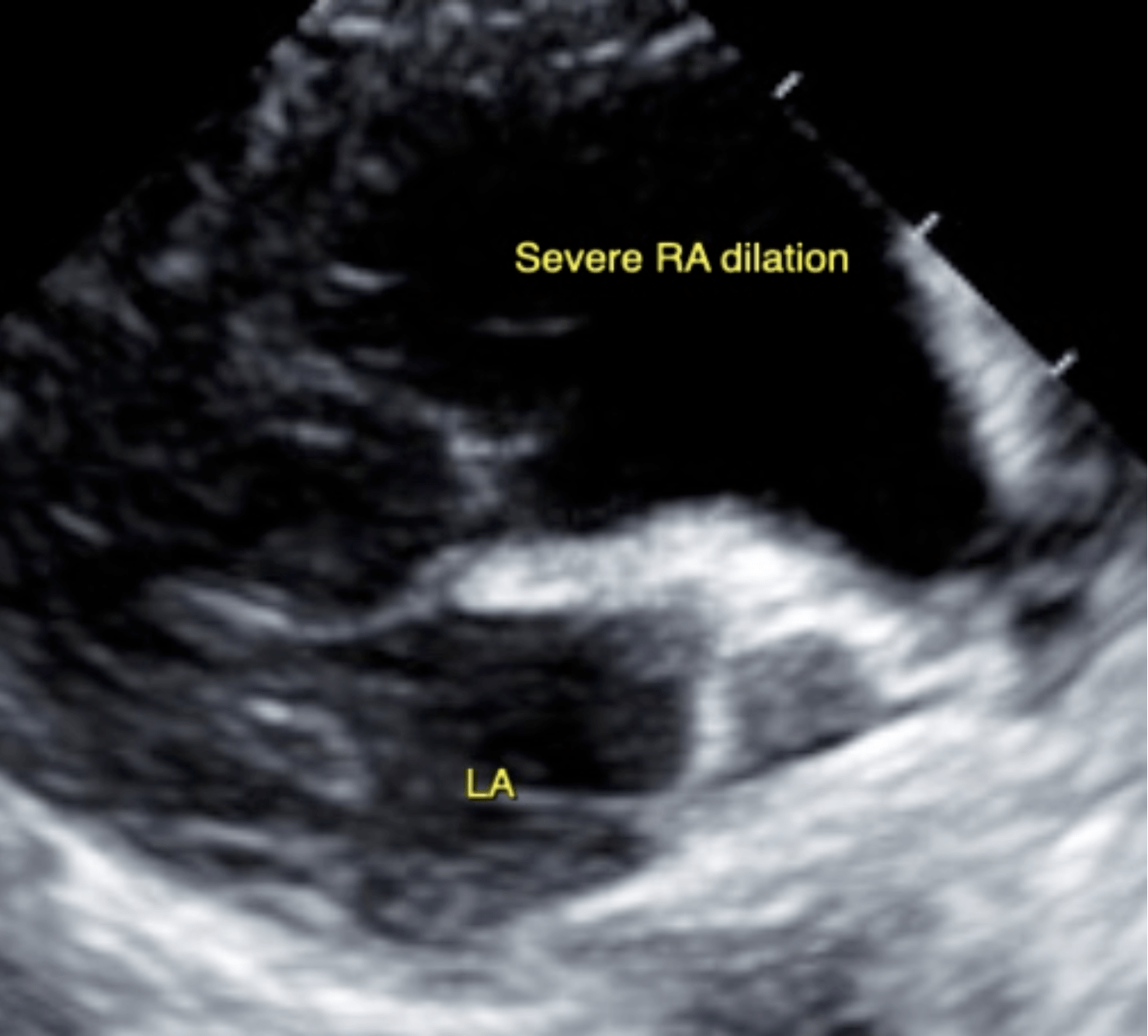
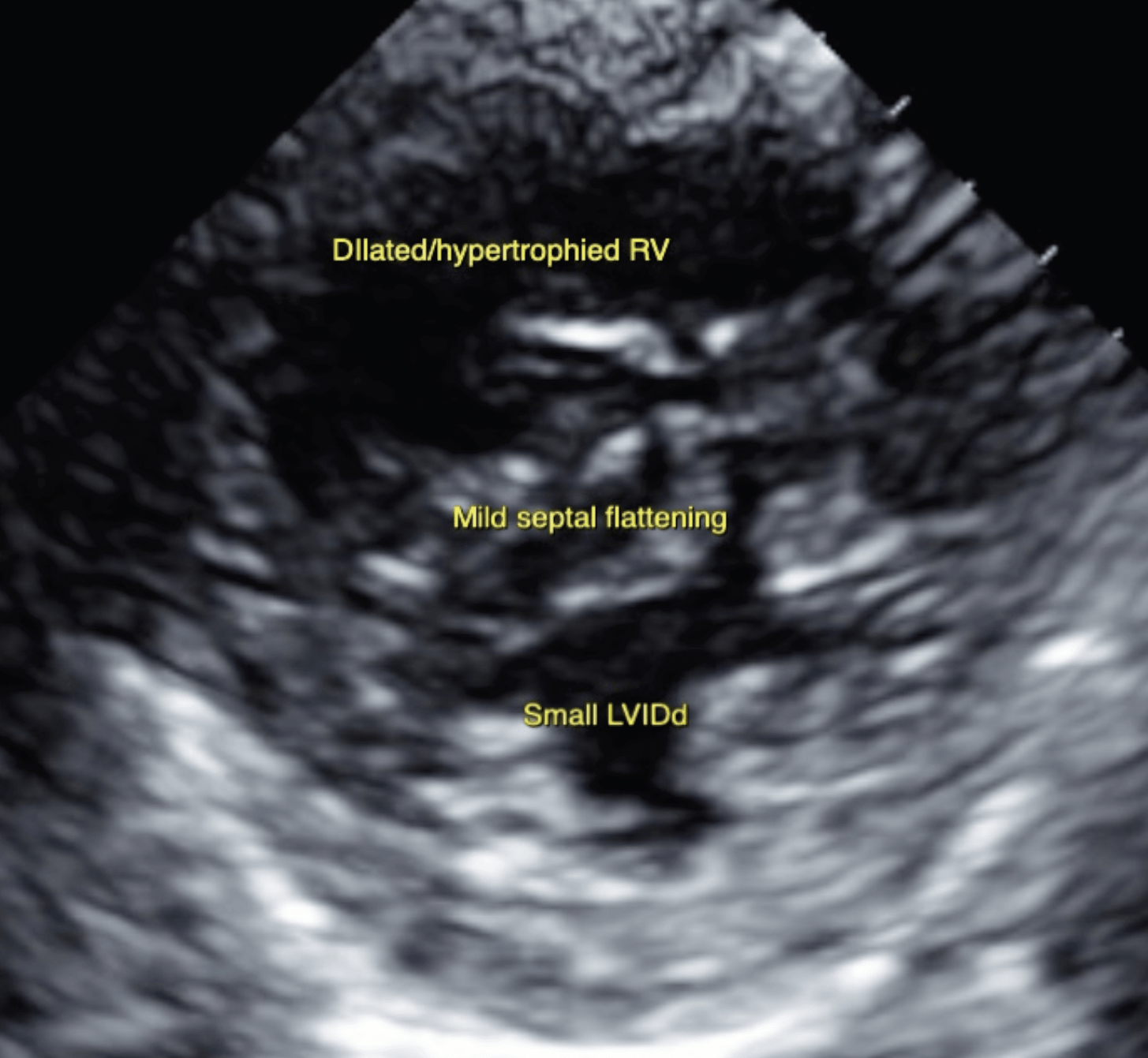
Severe pulmonary arterial hypertension with severe TR and right heart compensatory changes. Suspect primary respiratory crisis (infectious v inflammatory v PTE). Historical chronic airway disease. Mild MR with normal left heart dimensions.
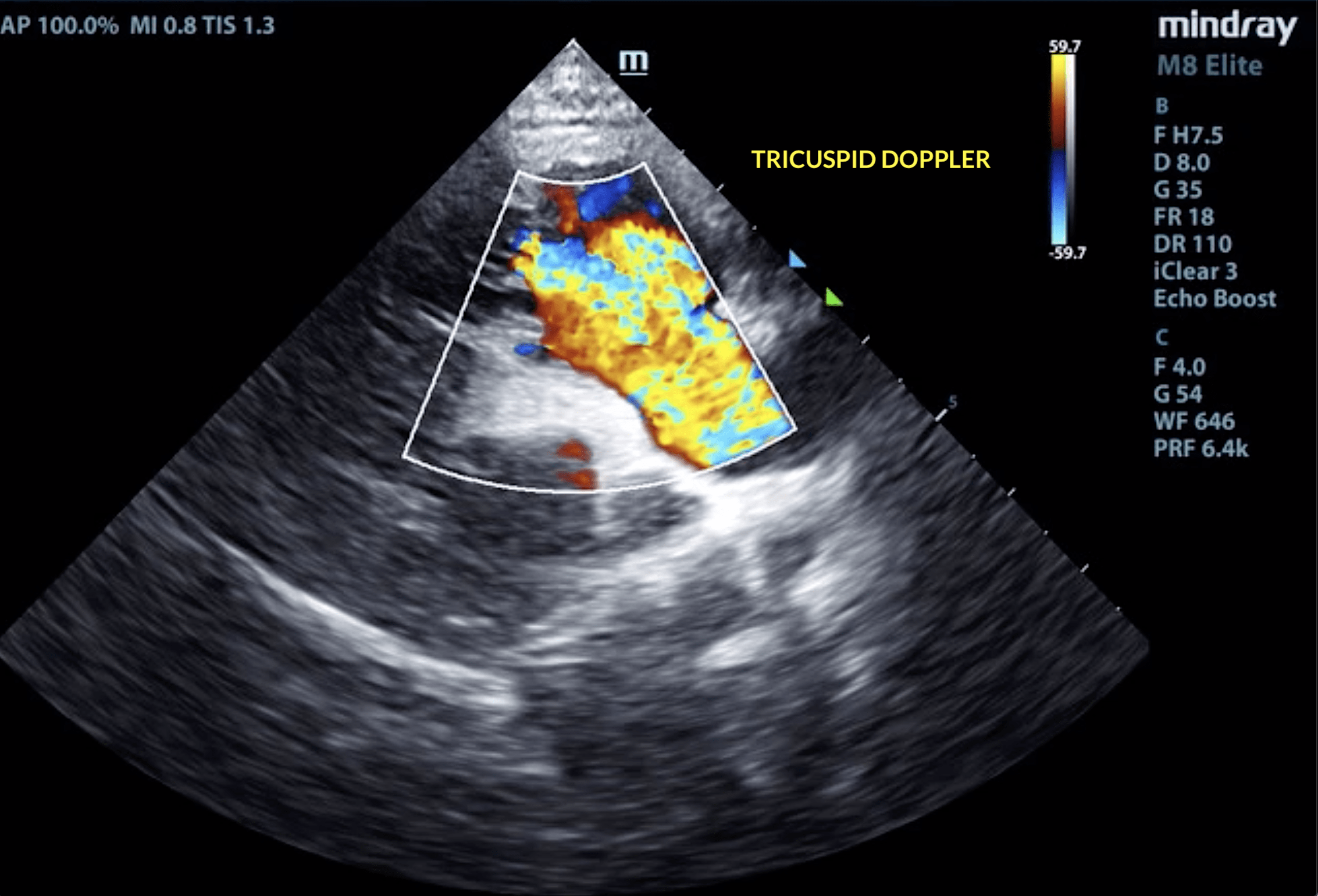
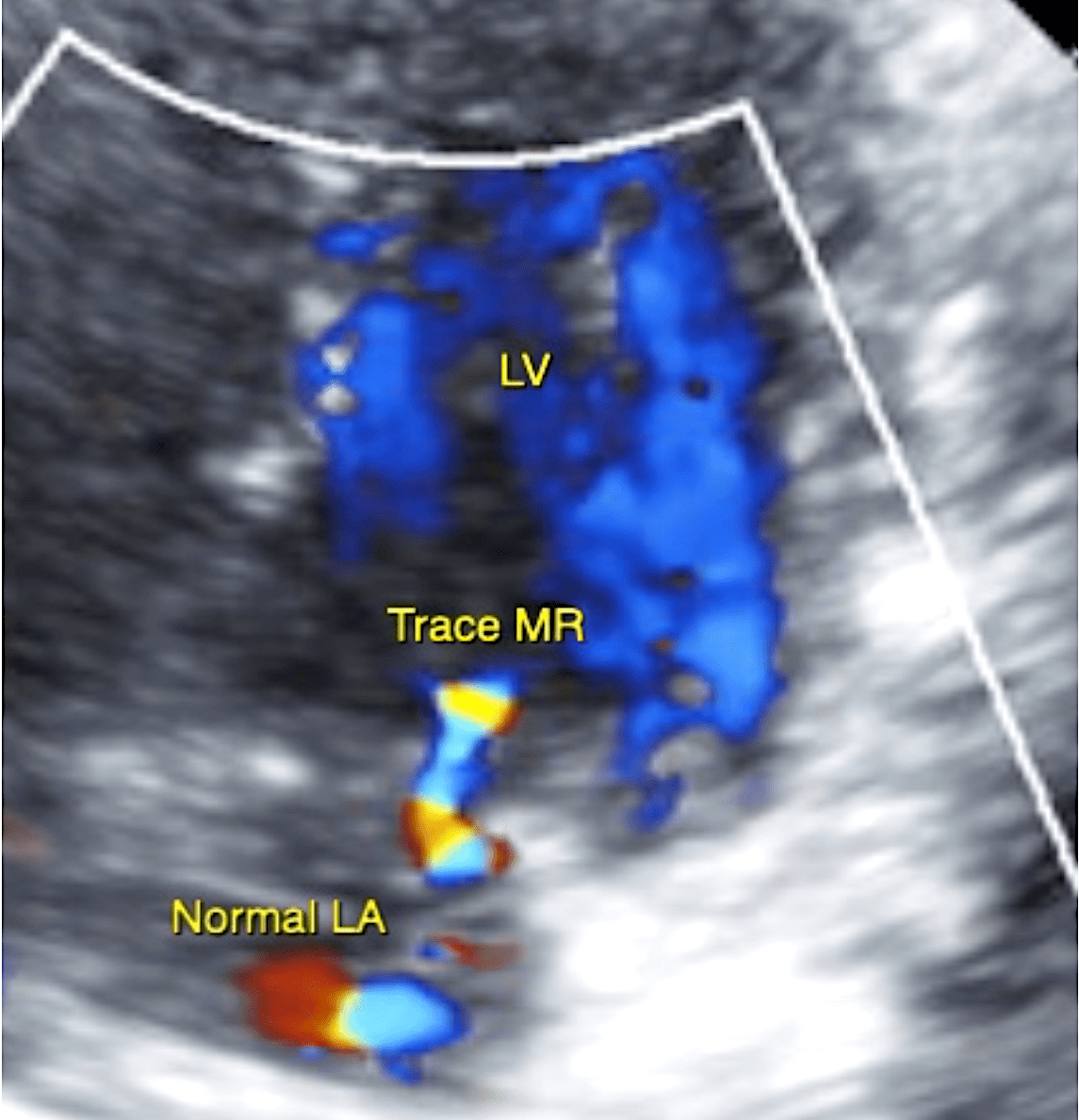
Diffuse thickening of mitral valve leaflets with no obvious prolapse into the left atrial lumen. Trace mitral regurgitation with normal left atrial dimension. Small LV diameter with adequate myocardial function and evidence of pseudohypertrophy. The tricuspid valve appears thickened and prolapsing, and there is severe tricuspid regurgitation. Severe right atrial enlargement; significant right ventricular dilation and hypertrophy consistent with severe pulmonary arterial hypertension. Systolic flattening of the IVS consistent with pressure overload. TR velocity consistent with pulmonary pressure gradient >90mmHg. The pulmonic and aortic valves are normal in morphology and mobility. Moderate MPA and branch dilation. No obvious pulmonic insufficiency. Normal pulmonic and aortic outflow velocities. Trace AI. No pericardial or pleural effusion noted. No cardiac tumors observed.
Diuretic was discontinued. Radiologist review was recommended. Institute pulmonary antibiotics (Enrofloxacin 5-7mg/kg PO q24h for 10+ days) +/- oxygen for supportive care. Institute sildenafil (Viagra) 20mg tablets, give ¼ tab PO q8h. Coontinue Pimobendan 1.25mg PO q12h. Depending on response/stability, can also consider bronchodilator such as theophylline, aminophylline, etc. Can also use hydrocodone and/or theophylline depending on chronic clinical signs of cough/exertional dyspnea. Recommend recheck echocardiogram in 4 months to reassess pulmonary pressures, sooner if any development of clinical signs.