This 8 year old MN Jack Russull Terrier dog initially presented with abdominal distension and ascites. Chemistry revealed low total protein at 4.2, low albumin at 1.9, phosphorus low at 1.0, calcium low at 8.1, cholesterol was high at 332. Urine protein to creatinine ratio was high at 5.4, microalbuminuria was high at >30. Urinalysis reveled protein of 3+, blood 1+ and transitional epithelia elevated at 2-3.
This 8 year old MN Jack Russull Terrier dog initially presented with abdominal distension and ascites. Chemistry revealed low total protein at 4.2, low albumin at 1.9, phosphorus low at 1.0, calcium low at 8.1, cholesterol was high at 332. Urine protein to creatinine ratio was high at 5.4, microalbuminuria was high at >30. Urinalysis reveled protein of 3+, blood 1+ and transitional epithelia elevated at 2-3.
Initial exam revealed slight small intestines due to inflammatory bowel disease, lymphangectasia, lymphoma or edema.
Differential diagnosis for ascites include right sided heart failure, portal hypertension, hypoalbuminemia, pancreatitis, peritonitis, uroabdomen, hemoabdomen, and neoplasia.
The appearance of the pancreas can be due to nodular hyperplasia, aging changes, pancreatitis, edema and neoplasia cannot be completely excluded.
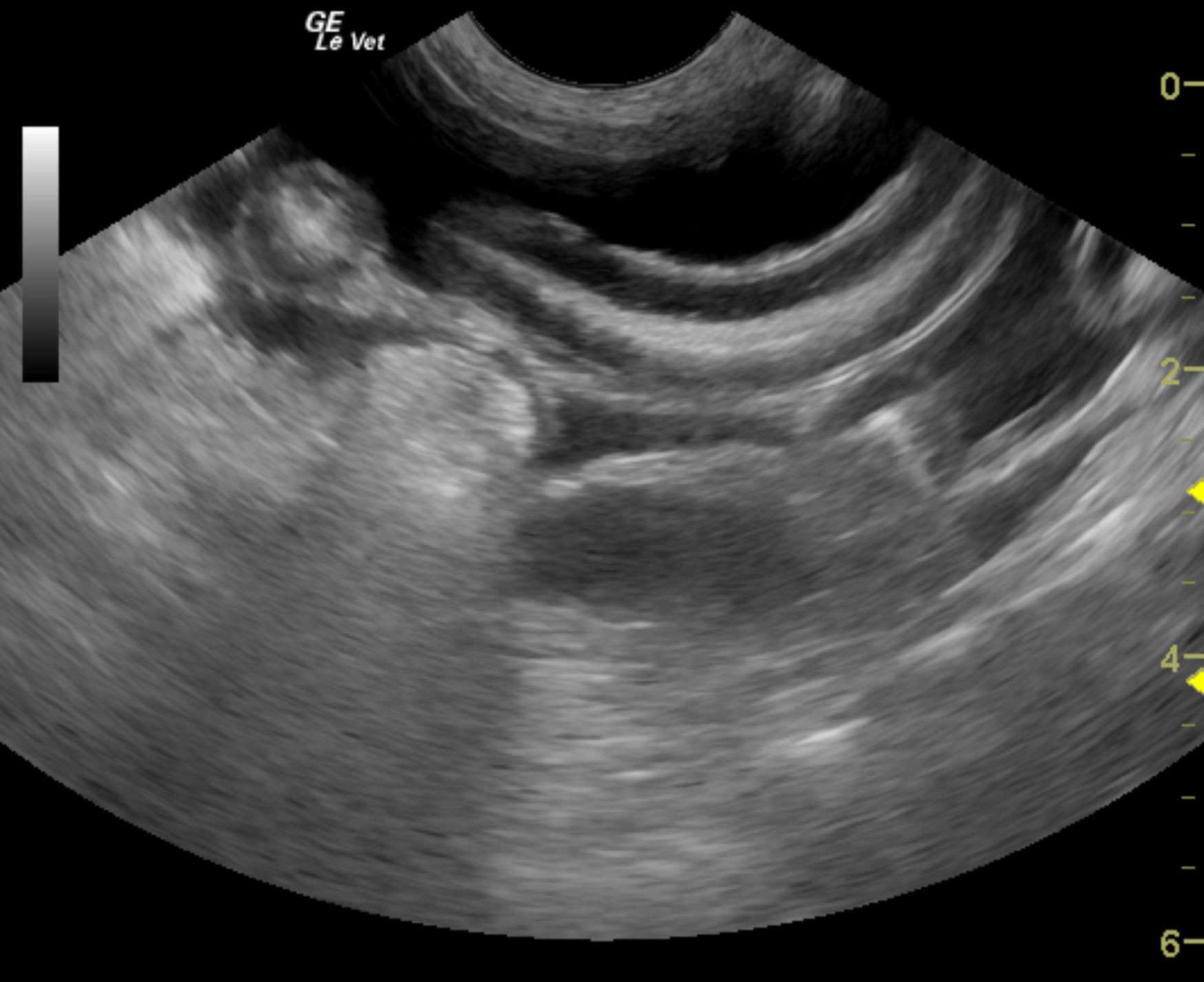
On initial ultrasound the patient had a large amount of ascites. The left kidney measured 4.38 cm and the right kidney measured 4.29 cm, both normal in size. Renal cortical echogenicity was normal as is the corticomedullary distinction. The small intestinal walls were slightly thickened and measured between 0.42-0.47 cm with normal wall differentiation. Slight mucosal stippling was noted as well. The area of the left pancreatic limb was normal in appearance but the right pancreatic limb was slightly mottled with a subtle nodular appearance, but no evidence of larges masses were seen. This area measured 4.08 x 1.51 cm.
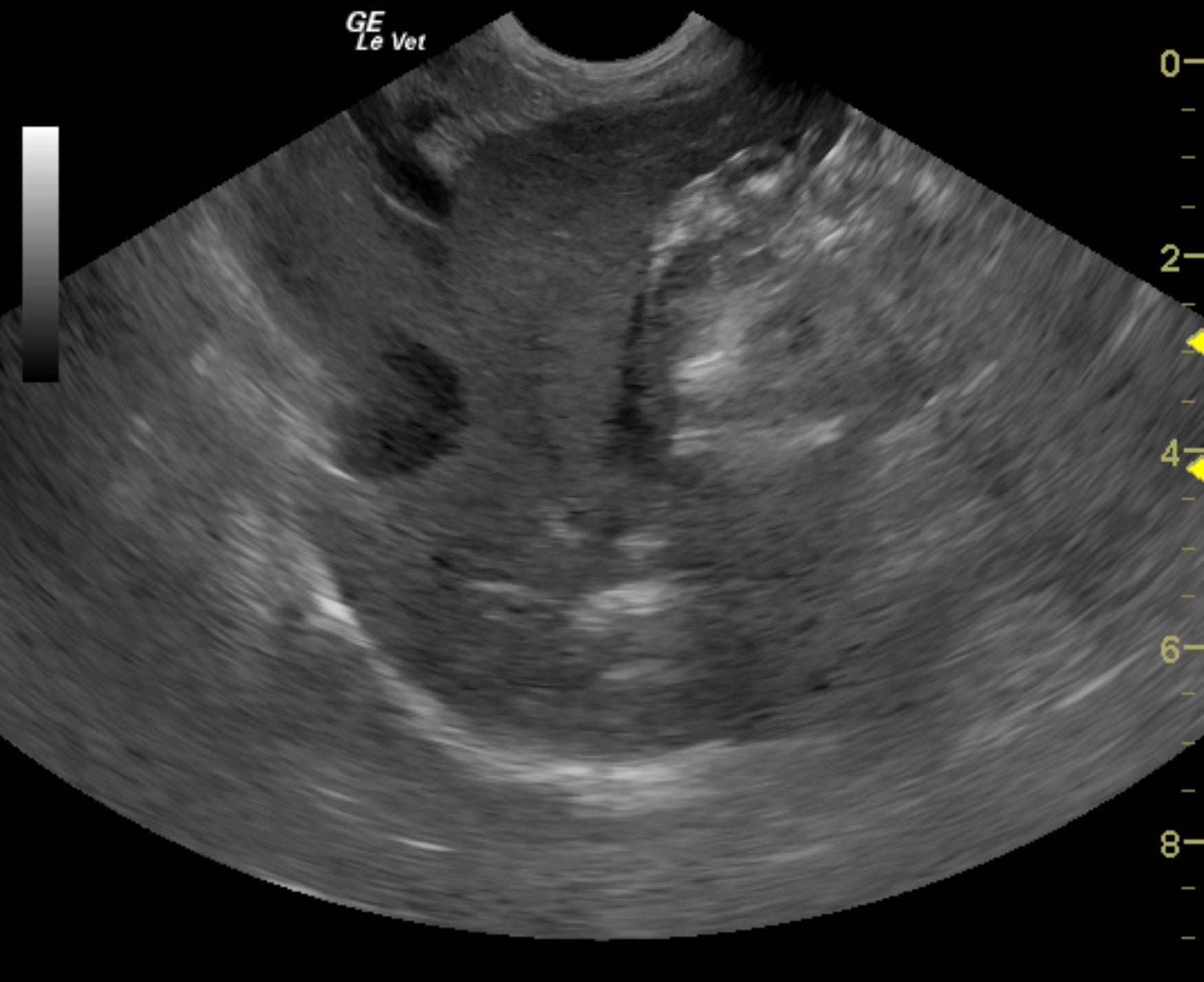
Repeat exam 3 weeks later revealed complete resolution of the ascites with normal portal vein velocity at 22 cm/sec. The vena cava revealed reduction of the tissue structure now confirmed to be thrombus and measured 2.69 x 0.46 cm with bloodflow that appears to tap around the thrombus in the vena cava at the diaphragmatic inlet.
Repeat ultrasound examination 5 weeks later revealed persistent, minor, degenerative renal changes with hypervascular cortices. This is consistent with protein losing nephropathy. Minor mineralization was noted in both kidneys, yet non obstructive. The remainder of the abdomen was unremarkable without progression. Thrombus noted on the prior sonogram in the vena cava appears to have completely resolved on the Plavix/aspirin combination.