“Well that’s not supposed to be there”…. mass in the left cranial abdomen. The sonogram defines if the lesion includes “crucial parts” or “extra parts” to remove. Define the lesion with a needle and remove it with a scalpel. Dx efficiency at its finest with unfortunately an inopportune outcome. Rachel Brilhart, RDMS of Intrapet Imaging in Baltimore, MD defines this pancreatic mass prior to surgery.
A 16-year-old FS DSH cat with history of diabetes and hyperthyroidism was presented due to vomiting, diarrhea, and anorexia. Physical exam found poor body condition and weight loss. Urinalysis showed SG of 1.017, proteinuria, and hematuria. A coagulation panel was mildly elevated.
A 16-year-old FS DSH cat with history of diabetes and hyperthyroidism was presented due to vomiting, diarrhea, and anorexia. Physical exam found poor body condition and weight loss. Urinalysis showed SG of 1.017, proteinuria, and hematuria. A coagulation panel was mildly elevated.
Pancreas clinical signs- pancreatitis, neoplasia, abscessation. Uncontrolled hyperthyroidism. G.I. clinical signs- IBD, neoplasia, intussusception, foreign body, ulceration, infectious (viral/bacterial/parasites). Renal clinical signs- renoliths, neoplasia. Interstitial cystitis.
Poorly differentiated adenocarcinoma. (Spleen and adhered omentum with no recognizable pancreatic tissue present).
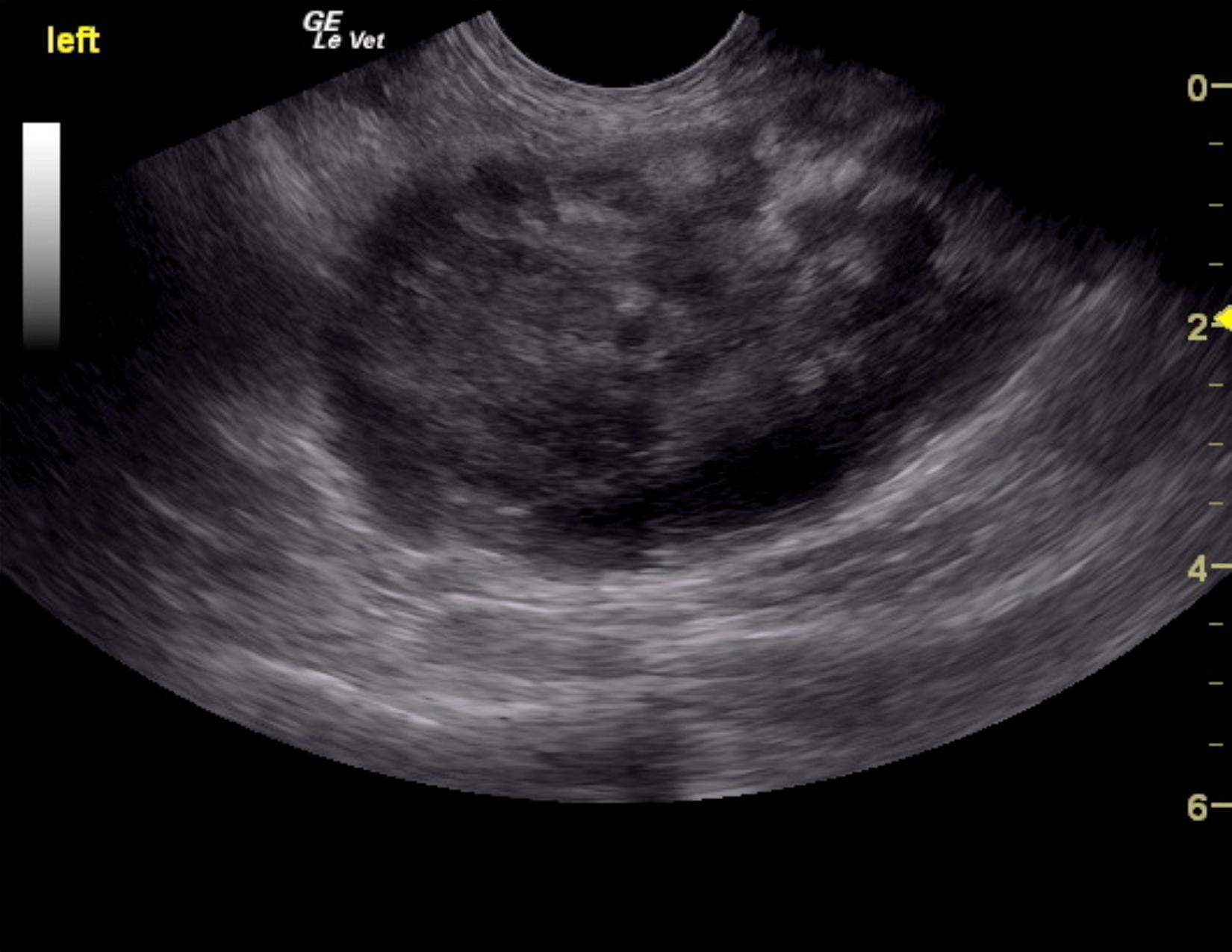
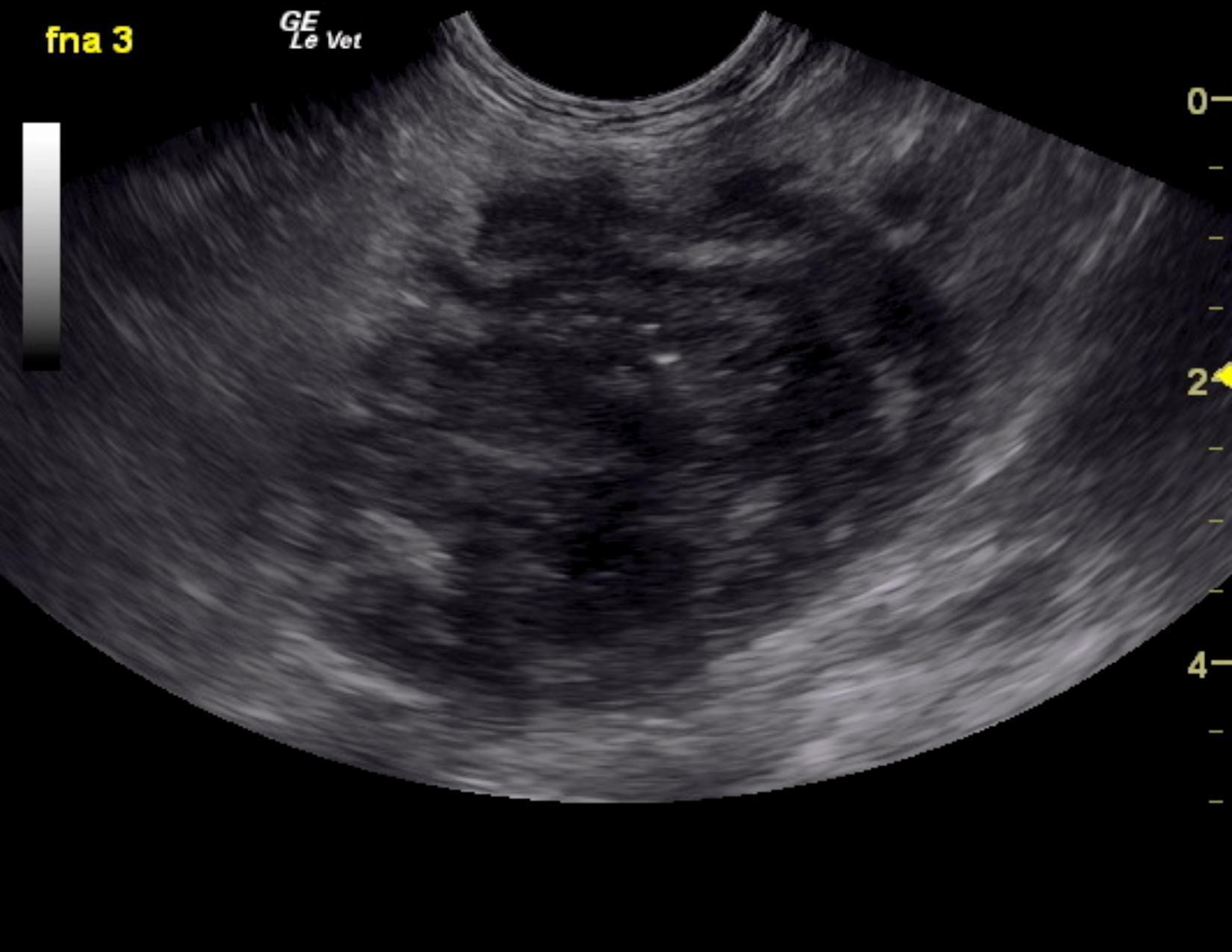
A left, caudal pancreatic mass was noted in this patient and measured 4.0 cm with moderate complexity attached to the left lobe of the pancreas. Hyperechoic surrounding fat was also noted. This is consistent with extension of the neoplastic process or associated inflammation. This appears potentially resectable. An exploratory surgery is recommended with removal of the adjacent lymph node measuring 1.5 cm (Not seen in these images). The right limb of the pancreas was mildly heterogenous, yet unremarkable. There was no overt evidence of metastatic disease noted. FNA was obtained of the pancreatic mass. The pancreas in this patient presented severely dilated duct at 0.49 cm with heterogenous, irregular parenchymal changes and tortuous pancreatic duct. The caudal abdomen revealed a cystic or irregular lymph node that measured 1.48 x 1.15 cm. This is likely jejunal lymph node with distorted architecture. Granulomatous disease or possible neoplasia may be present. FNA was recommended.
Clinical recommendations included chest radiographs, assessment of the cytology followed by exploratory surgery with aggressive left pancreatectomy as well as exploration for any evidence of metastatic disease that was not noted on ultrasound. However, no metastatic disease was overtly suspected and the lesion appeared to be largely isolated to the left pancreatic limb with minor capsular escape. Pancreatic carcinoma was the primary differential, however a granulomatous lesion was also a possibility from a sonographic aspect though less likely. The patient underwent exploratory surgery. The lesion was resected surgically even though it was wrapped around the splenic vessels. A concurrent splenectomy was also performed. The patient unfortunately died suddenly post-op after succesful resection. Thromboembolic episode was suspected.