3 year old MN DSH indoor only cat presented for PU/PD, smaller than normal stools and weight loss. Bloodwork performed in October 2011:
-Crea 298 (71-212)
-Ca 295 (195-283)
-T4 and CBC normal, FeLeuk/FIV negative
-Urine SG 1.022
-Culture negative
November 2011:
-Crea 294 (71-212)
– Ca 288 (195-283)
3 year old MN DSH indoor only cat presented for PU/PD, smaller than normal stools and weight loss. Bloodwork performed in October 2011:
-Crea 298 (71-212)
-Ca 295 (195-283)
-T4 and CBC normal, FeLeuk/FIV negative
-Urine SG 1.022
-Culture negative
November 2011:
-Crea 294 (71-212)
– Ca 288 (195-283)
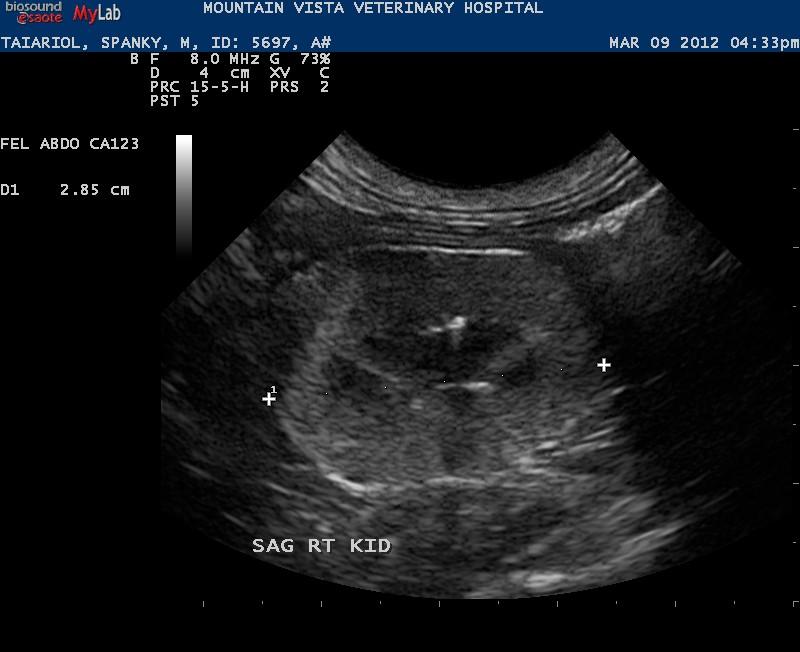
X-rays showed the presence of renoliths and a size discrepency in kidneys.The owner went away, as pet was stable, but cam home to find that the pet has lost more weight, still is PU/PD and being picky with his diet. She came to my hospital for a second opinion. We re-ran bloowork (results pending) and collected urine via cystocentesis SG 1.023, no evidence of infection on sediment but few RBC’s – culture pending – did not run pro:crea ratio due to presence of blood. Abdominal ultrasound showed renoliths in both kidneys and a small right kidney. The rest of the abdomen was unremarkable and there was no evidence of obstructive kidney disease (ureters not seen, urinary bladder normal). We are having the owner back when pet is fasted to run a hypercalcemia of malignancy panel.
I am thinking possible idiopathic hypercalcemia causing renoliths and renal failure or renal dysplasia due to the age of this patient. What do you think of these kidneys?


12 responses to “Renoliths, hypercalcemia and azotemia”
Wow, the x-ray came out
Wow, the x-ray came out really distorted – sorry about that!
Jacquie
Wow, the x-ray came out
Wow, the x-ray came out really distorted – sorry about that!
Jacquie
Hi Jacquie, please try to
Hi Jacquie, please try to keep the concise bullet format to be consistent. Looks like its one of those periodic stone movers. Large infarct cranial pole of both kidneys and small stones that are not obstructiong now but have been before and will in the future. Stone passage and temporary hydroureter/hydronephroisis sometimes we dont catch but can only surmise by the sono-clinical scenario. This is likely one of those cases and the kidneys , via infarction and fibrosis, passage by passage waste away and shrivel up which explains the disparity in size.
Eric
Hi Jacquie, please try to
Hi Jacquie, please try to keep the concise bullet format to be consistent. Looks like its one of those periodic stone movers. Large infarct cranial pole of both kidneys and small stones that are not obstructiong now but have been before and will in the future. Stone passage and temporary hydroureter/hydronephroisis sometimes we dont catch but can only surmise by the sono-clinical scenario. This is likely one of those cases and the kidneys , via infarction and fibrosis, passage by passage waste away and shrivel up which explains the disparity in size.
Eric
Also, the ill-defined fat in
Also, the ill-defined fat in the LK pelvis would make me suspect active inflammation as well as those stones are in position to move into the ureter. Judging by the clean aspect of the stones I would suspect oxalates but this is just an educated guess.
Eric
Also, the ill-defined fat in
Also, the ill-defined fat in the LK pelvis would make me suspect active inflammation as well as those stones are in position to move into the ureter. Judging by the clean aspect of the stones I would suspect oxalates but this is just an educated guess.
Eric
Eric
The large infarcts you
Eric
The large infarcts you are referring to, are they the hyperechoic regions in the cortices? Do infarcts remain permanent lesions in the kidneys?
Jacquie
Eric
The large infarcts you
Eric
The large infarcts you are referring to, are they the hyperechoic regions in the cortices? Do infarcts remain permanent lesions in the kidneys?
Jacquie
Yes that is correct. It hasnt
Yes that is correct. It hasnt been studied well but my thinking on this is the stone passage causes hydronephrosis then cortical hypoxia likely occurs and then infarctions which, when acute are hypo to isoechoic owing to edema and inflammation and then when they fibrose they retract the capsule and become hyperechoic owing to scar tissue. the classic one is a triangle but they can take many shapes. I have seen them in cases of nephrolithiasis, pylelonephritis, hypertension….anything that causes a local virchow’s triad i think would justify infarctions…infectious disease…
maybe remo and marty can add to this..
Eric
Yes that is correct. It hasnt
Yes that is correct. It hasnt been studied well but my thinking on this is the stone passage causes hydronephrosis then cortical hypoxia likely occurs and then infarctions which, when acute are hypo to isoechoic owing to edema and inflammation and then when they fibrose they retract the capsule and become hyperechoic owing to scar tissue. the classic one is a triangle but they can take many shapes. I have seen them in cases of nephrolithiasis, pylelonephritis, hypertension….anything that causes a local virchow’s triad i think would justify infarctions…infectious disease…
maybe remo and marty can add to this..
Eric
I would be concerned for
I would be concerned for hypercalcemia of malignancy in this patient with secondary renal disease from the hypercalcemia. Although primary renal disease (pyelonephritis, dysplasia, chronic kidney disease) can result in hypercalcemia it is usually evident with advanced disease, which this cat does not seem to have (creatinine only 1.5 times elevated, no anemia). Idiopathic hypercalcemia is possible but only a rule out diagnosis. If possible get an ionized calcium done as it is often out of proportion high in cats with idiopathic hypercalcemia.
I would be concerned for
I would be concerned for hypercalcemia of malignancy in this patient with secondary renal disease from the hypercalcemia. Although primary renal disease (pyelonephritis, dysplasia, chronic kidney disease) can result in hypercalcemia it is usually evident with advanced disease, which this cat does not seem to have (creatinine only 1.5 times elevated, no anemia). Idiopathic hypercalcemia is possible but only a rule out diagnosis. If possible get an ionized calcium done as it is often out of proportion high in cats with idiopathic hypercalcemia.